Most head and neck cancers are preventable, however, more than 15,500 cancer deaths each year are due to smoking, sun exposure, poor diet, alcohol, inadequate exercise or being overweight.
The most preventable cause of cancer is smoking - which directly causes more than 11,000 new cases of cancer each year, that is 12.5% of all new cases of cancer. Cancer of the mouth is the 6th largest cause of mortality in males according to the NSW Cancer Council statistics.
Quit smoking - your health and your budget will benefit. If you are a non-smoker, limit your exposure to other people's smoke.
Early detection of Head and Neck Cancer
Cancer of the head and neck is usually curable if caught early. Fortunately, most head and neck cancers produce early symptoms.
Some symptoms of head and neck cancer are:
- a lump in the neck.
- change in the voice.
- a growth in the mouth (an ulcer in the mouth).
- bleeding.
- pain.
- swallowing problems.
- changes in the skin.
- persistent earache.
If any of these symptoms last more than two weeks you should be seen by your GP as soon as possible.
If your GP is concerned he or she will then refer you to see one of our Oral and Maxillofacial Surgeons. Of course not all lumps, changes in the voice or any of the above symptoms are cancer so it is best to seek the advice of your GP before you become concerned.
How is Oral Cancer diagnosed?
When coming to our surgery for concerns relating to oral cancer our surgeons will do one or more of the following examinations.
- biopsy - tissue samples are taken by using a variety of instruments. The surgeon will send the tissue to a pathologist, a specialist in the diagnosis of abnormal tissue, who can also assess whether the tissue is non-cancerous (benign) or cancerous (malignant). The pathologist will then send a report to the surgeon, who will discuss the findings and options for further treatment with the patient. In some cases, a second biopsy may be needed to further refine the diagnosis.
- Computed Tomography (CT or CAT scan) - this is a non-invasive procedure that takes cross-section images of the head and neck or other internal organs. This is then used to detect any abnormalities that may not show on an ordinary x-ray taken by your dentist or GP.
- Ultrasonography (Ultrasound) - this technique uses high-frequency sound waves to create an image of the internal organs.
Magnetic Resonance Imaging (MRI) - this type of imaging produces a two or three dimensional view of a particular internal organ or structure.
Once a diagnosis is made your surgeon will determine the type of treatment you require.
Treatment
Treatment for oral cancer depends on a few factors:
- your age, overall health and medical history
- extent of the disease
- your tolerance for specific medications, procedures, or therapies
- expectations for the course of the disease
- your opinion or preference
Types of treatment
- surgery there are different types of surgery specific to different types of cancer, these include:
- primary tumour resection - this requires the removal of the entire tumour and surrounding area of tissue. In most cases this can be done through a biopsy for small cancers. For large cancers patients require major surgery.
- maxillectomy - this requires removal of the tumour, part or all of the hard palate (roof of the mouth) and bone if necessary.
- mandibulectomy - this requires partial or total removal of the lower jaw.
- laryngectomy - this is for the removal of a large tumour of the tongue or oropharynx, if it extends to the larynx (voice box). This is done in association with an ENT Surgeon.
- neck dissection - this type of surgery is necessary if the cancer has spread to the lymph nodes in the neck. The lymph nodes may also need to be removed.
- radiation therapy - this is a type of treatment sometimes used in conjunction with surgery. It uses high-energy rays to damage the cancer cells. This method of treatment assists in minimising the spread of the cancer.
- chemotherapy - this is medication that affects cancer cells. It has the ability to interfere with cancers cell replication. It can be used in combination with both surgery and radiation therapy.
How to prepare for surgery
Usually, a biopsy of the suspected tumour would be performed to verify and establish the final diagnosis. This may be done under local anaesthesia or under general anaesthesia in day surgery. Once the diagnosis is confirmed, patients would be referred to Hospital for further treatment.
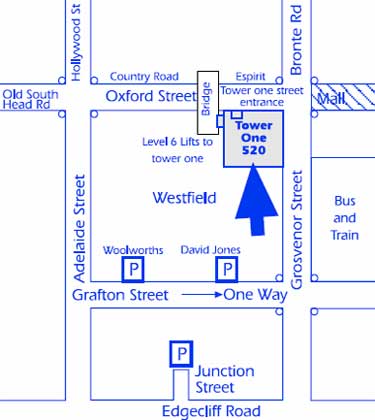
- Randwick Day Surgery or Eastern Suburbs Private Hospital for minor procedures or
- St Vincent's Private Hospital, Darlinghurst or Prince of Wales Hospital, Randwick for more complicated cases.
A choice of these two hospitals depends upon:
- whether you have private hospital cover; and
- if you don't have private hospital cover you will more than likely have to go on the public waiting list as a priority patient or pay full price.
You may also be referred to other specialists to help with your treatment.
When booking in for surgery you will be informed of the type of surgery you will be having, what to expect following your surgery, how to manage your pain and the risks and benefits associated with your surgery.
You will also be given ample opportunities to ask any questions regarding your surgery or any concerns you may have. You are also welcome to contact our consulting rooms if you have any further questions.
Side Effects
Depending on the type of surgery performed there are some known and predictable temporary side effects.
- pain - it is not uncommon to experience pain following your surgery. Appropriate analgesics (pain killers) are given to you in hospital to comfortably manage your pain. Upon discharge you will also be provided with analgesics to take home.
- swelling - on the face commences immediately after surgery and reaches a peak at about 48 hours. It does not begin to decrease significantly for about one week after the operation.
- sore mouth/surgical site
- difficulty chewing, talking or swallowing
- fatigue
- nausea
- vomiting
- mouth sores
- lack of appetite
Rehabilitation
Rehabilitation varies from person to person, the type of surgery performed, the location and extent of cancer. Rehabilitation may include:
- dietary changes - after surgery some patients may have difficulty eating, it is recommended that you eat small, soft, moist meals.
- follow up surgery - depending on the type of surgery performed it may be a benefit to some patients to have reconstructive or plastic surgery to restore the surgical site.
- prosthesis - prosthetics are another option to reconstructive and plastic surgery.
- speech therapy - speech therapy may be needed to help a patient having difficulties with speech after some of the major cancer surgeries.
Any surgical or invasive procedure carries risks. Before proceeding, you should seek a second opinion from an appropriately qualified health practitioner.